Table of Contents
Vaginas & Sex After Giving Birth
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Apr 11, 2023

Natural labor and childbirth are intrinsic processes that, under the best of normal and uncomplicated circumstances, result in the delivery of an infant by passage through the “birth canal,” or the vagina. The pregnancy journey and giving birth are monumental life events that lead to many changes, especially to the birthing person’s body. For persons with a female reproductive health system, the vagina can undergo significant stretching during childbirth, leading to various issues, such as vaginal infections, tearing, discharge, dryness, and changes in sexual function. In this article, we'll explore some of the most common questions and concerns surrounding vaginal health and sex after giving birth.
Are you more susceptible to vaginal infections during or after pregnancy?
The short answer is yes. Pregnancy and childbirth can affect the balance of bacteria in the vagina, leading to an increased risk of infections. During pregnancy, the hormonal changes that occur can cause the vaginal pH to become more alkaline, which can encourage the overgrowth of naturally occurring yeast and/or bacteria. Additionally, the increased blood flow to the pelvic region during pregnancy can make the vaginal tissues more susceptible to infection by further disrupting the pH balance. Research has also demonstrated that the microbiome of pregnant people differs from that of non-pregnant people with a female reproductive system. Yeast infections are generally not considered harmful during pregnancy and have no effect on the baby's development, but numerous studies have shown an association between bacterial vaginitis (BV) and preterm labor or even preterm delivery.
After giving birth, the risk of infection increases even further. The vagina's natural defenses are weakened after birth during the inflammatory healing process. The pH balance is further disrupted in the postpartum weeks by the natural passage of lochia or menstrual-like bleeding, which is the shedding of the uterine lining that helped support the pregnancy process. Additionally, the presence of any tears or even small cuts in the vaginal mucosa can also provide a gateway for bacteria to prolong the inflammation state.
How often do tears occur during birth?
Research studies have found that the pelvic floor tissues can stretch more than three times their normal length during a vaginal birth due to the flexibility enabled by the pregnancy hormone state. Despite this natural ability, 53-79% of patients experience some degree of tearing, or vaginal lacerations, during vaginal birth, according to the American College of Obstetricians and Gynecologists (ACOG). The rate of tearing during childbirth varies widely as its occurrence depends on a range of factors, such as the baby's size, the length of labor, the individual’s pelvic muscle anatomy, and the use of delivery assistance instruments like forceps or a vacuum.
Most tears are minor and heal on their own, but more severe tears may require stitches or other medical interventions. It is important to talk to your prenatal care clinician about your personalized risk of tearing and what steps you can take to reduce the likelihood.
What can you do to avoid tearing?
Tearing is a common concern for many patients during childbirth. Fortunately, there are steps that you can take to help reduce the likelihood, or at least the degree, of laceration. One of the most effective ways to avoid or minimize tearing is to prepare your body for childbirth. This involves exercising during pregnancy to strengthen the pelvic floor muscles. Exercises, such as Kegels or squats, as well as maintaining an active lifestyle by integrating daily walks, prenatal yoga or even regular stretching have been shown to help reduce the risk of lacerations and improve the labor process. ACOG guidelines also indicate that perineal massage to help stretch the vaginal tissues starting at around 8 months was associated with a modest reduction in lacerations requiring stitches.
During labor, your healthcare provider can also take steps to minimize tearing. They may use perineal massage or warm compresses to help stretch the vaginal tissues and reduce the risk of tearing. In some cases, an episiotomy may be performed, which involves making a small incision under local anesthesia at the vaginal opening to help prevent unpredictable tears and create more room for the baby to be delivered.
It is important to note that tearing is a common occurrence during childbirth, and it's not always possible to avoid it entirely. However, taking steps to prepare your body and working with your clinician can help reduce the risk.
"Will I be loose after having a baby?"
The idea that giving birth will cause a woman's vagina to become "loose" is a common misconception. While it's true that the vaginal tissues can stretch significantly during childbirth, this does not necessarily mean that the vagina will remain permanently stretched or become "loose." Research studies have found that while patients who had vaginal deliveries had wider vaginal openings than those who had never given birth, there was no significant difference in vaginal laxity or tightness between the two groups. Additionally, the same study found that patients who practiced pelvic floor muscle exercises had better muscle tone and less pelvic floor dysfunction than those who did not.
It's important to note that each body is unique, and some may experience vaginal tightness or muscle tone changes after giving birth. However, you can take steps to support vaginal health and pelvic floor strength, such as practicing Kegels or other pelvic floor exercises as discussed earlier.
What are expected postpartum discharge and vaginal changes?
After giving birth, many patients may experience varying amounts of postpartum bleeding or discharge, known as lochia. This discharge is a combination of blood, vaginal mucus, and uterine lining tissue that can last several weeks after giving birth. It's essential to practice good hygiene during this time, such as changing pads frequently and avoiding tampons as well as anything else inside the vagina, to help reduce the risk of vaginal infections and ensure proper healing of any tears that may have occurred.
There are three general stages of lochia:
- Lochia Rubra: Within the first week of giving birth, it appears very similar to a heavy period with dark or bright red blood and even small clots with mild cramping. The bleeding should never exceed two fully-soaked pads in 1 hour, and any patient experiencing this degree of bleeding should present to an emergency room for further assessment and treatment.
- Lochia Serosa: After the initial week or so after birth, the lochia becomes watery with a lighter red to brown or pink-brown tinge, a moderate flow, and little to no clots. This type of lochia can last up to 2 weeks for many patients.
- Lochia Alba: Finally, the lochia discharge becomes predominantly light yellow to white, with very little blood or spotting present. This final stage can persist for approximately six to eight weeks after birth.
The color, consistency, and duration vary by the individual, but some factors impact how much lochia you see. Physical activities, like walking or climbing stairs, may cause more to appear, especially if you were just sitting or lying down. Lactating and breastfeeding have also been found to increase the pattern and amount of lochia.
In addition to discharge, some may experience vaginal dryness after giving birth. This is due to hormonal fluctuations after pregnancy which cause a temporary decrease of estrogen in the body. Lactation can also suppress estrogen levels compounding this issue. Vaginal dryness from this temporary low estrogen state can cause discomfort during sex, as well as itching or burning, which may impact sexual desire.
Do you experience low sexual desire after giving birth?
Low sexual desire or libido is a common issue that many people may experience after giving birth. There are several factors that can contribute to this, including fatigue, hormonal changes, physical discomfort, and the demands of caring for a newborn.
A study published in the Journal of Sexual Medicine found that women's sexual desire decreased significantly in the first three months after giving birth but then gradually increased over time. However, it's important to note that every person's experience is different, and some may have a more prolonged decrease in libido.
If you're experiencing low sexual desire after giving birth, it's essential to talk to your healthcare provider about your concerns. They can help identify any underlying issues and provide recommendations for treatment or support.
Does sex feel different after giving birth?
As many patients report, sex can feel different after giving birth. The stretching and tearing of vaginal tissues during childbirth can cause changes in the way sex feels. Some may experience pain or discomfort during sex, while others may notice decreased sensitivity or changes in vaginal lubrication. Recent research has demonstrated that patients who had vaginal tears during childbirth were more likely to experience pain during sex in the postpartum period. However, the same study also found that those who practiced perineal massage before childbirth had lower rates of pain during sex. It's important to communicate with your partner and healthcare provider about any changes in how sex feels after giving birth. Your healthcare provider may be able to recommend treatments or strategies to help alleviate pain or discomfort during sex.
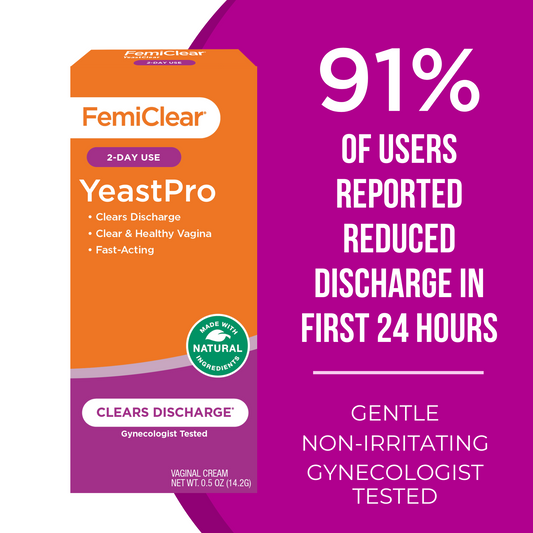
In conclusion, giving birth can significantly impact vaginal health and sexual function. Keep in mind that every person’s experience is unique, and there is no one "right" way to navigate postpartum vaginal health and sexuality. Good hygiene practices are key for vaginal health maintenance during and after pregnancy. By using naturally-derived products, like FemiClear’s Restoratives Feminine Wash and other vaginal health remedies, to help maintain pH balance as well as by taking essential steps to support your body during and after childbirth, such as preparing for labor and communicating with your clinician, you can optimize the factors influencing vaginal and sexual health postpartum.
References:
Shimaoka M, Yo Y, Doh K, Kotani Y, Suzuki A, Tsuji I, Mandai M, Matsumura N. Association between preterm delivery and bacterial vaginosis with or without treatment. Sci Rep. 2019 Jan 24;9(1):509.
Freitas AC, Chaban B, Bocking A, et al. The vaginal microbiome of pregnant women is less rich and diverse, with lower prevalence of Mollicutes, compared to non-pregnant women. Sci Rep. 2017;7(1):9212. Published 2017 Aug 23.
Romero R, Hassan SS, Gajer P, et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women [published correction appears in Microbiome. 2014 Apr 15;2(1):10]. Microbiome. 2014;2(1):4. Published 2014 Feb 3.
Prevention and management of obstetric lacerations at vaginal delivery. Practice Bulletin No. 198. American College of Obstetricians and Gynecologists. Sept 2018, reaffirmed 2022.
Ashton-Miller JA, Delancey JO. On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng. 2009;11:163-176.
Fletcher S, Grotegut CA, James AH. Lochia patterns among normal women: a systematic review. J Womens Health (Larchmt). 2012 Dec;21(12):1290-4. doi: 10.1089/jwh.2012.3668. Epub 2012 Oct 26.
Spaich S, Link G, Alvarez SO, et al. Influence of Peripartum Expectations, Mode of Delivery, and Perineal Injury on Women's Postpartum Sexuality. J Sex Med. 2020;17(7):1312-1325.
O’Malley, D., Higgins, A., Begley, C. et al. Prevalence of and risk factors associated with sexual health issues in primiparous women at 6 and 12 months postpartum; a longitudinal prospective cohort study (the MAMMI study). BMC Pregnancy Childbirth 18, 196 (2018).
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Apr 11, 2023
Soothing Feminine Wash
Daily relief from vaginal itching and irritation
Learn More