Table of Contents
Can Antibiotics Cause a Yeast Infection?
Oct 26, 2025

Experiencing oral thrush after a round of antibiotics? How about itching and swelling in the vaginal area? If so, you may have a yeast infection, a common but overlooked side effect of antibiotics.
Yeast infections (called vaginal candidiasis) are fungal infections that can affect the skin, mouth, digestive system, and reproductive system. They cause thick, cottage cheese-like discharge in the vagina as well as itchiness and irritation in the vagina and vulva.
Antibiotic use may increase your risk of developing a yeast infection. This article covers the connection between antibiotics and yeast infections, answering questions like can antibiotics cause a yeast infection, why do antibiotics cause yeast infections, and how to prevent a yeast infection while using antibiotics.
Understanding the Link
The link between antibiotics and yeast infections is strong yet often overlooked.
Every woman has small amounts of candida, the bacteria that causes yeast infections, inside their vaginas. It lives alongside other good and bad bacteria and yeast, making up what is called your vaginal flora or vaginal microbiome. This balance of good and bad bacteria and yeast in the vagina is essential for maintaining vaginal health.
Antibiotics kill off bad bacteria in the body to treat a bacterial infection, like strep throat or pneumonia. However, some antibiotics also kill off healthy bacteria, which can disrupt the body’s natural balance of bacteria and yeast. This disruption can cause candida overgrowth in the vaginal region and lead to a yeast infection.
Yeast infections don’t just occur in the vagina, however. They can also affect the skin, mouth, and digestive system. Oral yeast infections, or oral thrush, can cause creamy, white lesions on the tongue, inner cheeks, or gums. They may also cause pain or difficulty swallowing. Vaginal yeast infections cause thick, cottage cheese-like discharge in the vagina as well as redness, itchiness and irritation in the vagina and vulva.
Yeast infections due to antibiotics are more common than you might think. Infections can occur during or shortly after antibiotic treatment. Moreover, your individual health and the type of antibiotic you take can influence your risk.
How Antibiotics Trigger Yeast Infections
Antibiotics trigger yeast infections by essentially being too good at their jobs.
The vagina maintains its own balance of bacteria and yeast, known as the vaginal flora or microbiome. One type of bacteria, called Lactobacillus, creates a slightly acidic environment in the vagina which helps keep yeast growth in check.
Antibiotics are often needed to treat illnesses like sinus infections, strep throat, pneumonia, or bronchitis. These medications successfully kill off the bad bacteria that cause these infections. However, they may also wipe out good bacteria living throughout the entire body, not just the area it is treating, in the process.
Certain antibiotics can wipe out beneficial bacteria like Lactobacillus livingin the mouth or vagina. A lack of Lactobacillus creates an environment where candida can overgrow, causing an oral or vaginal yeast infection.
Common Symptoms to Watch For
Both oral and vaginal yeast infections can be a side effect of antibiotic use. Symptoms are often mild in both types of infections but can become severe in some cases. In addition, both oral and vaginal yeast infections typically require treatment with antifungal medications.
Many people suspect they have a vaginal yeast infection due to symptoms like itching and abnormal discharge. Sometimes it can be difficult to tell a yeast infection apart from other vaginal infections. If you are taking or have recently finished taking antibiotics, these are some symptoms to watch out for.
Signs of a vaginal yeast infection include:
- Thick, white discharge that resembles cottage cheese
- An itchy vulva or vagina
- Redness and swelling in vulva
- Burning while peeing
- Pain during sex
- Soreness and pain in vagina and vulva
- Rash
While less common, some people also experience lethargy, fever, and chills with vaginal yeast infections. This is likely due to the body’s response of fighting off the infection.
Signs of oral thrush or an oral yeast infection after antibiotic use include:
- Creamy white spots or patches on the tongue, cheeks, roof of mouth, gums, and tonsils
- Redness or burning in mouth and throat
- Difficulty eating or swallowing
- Cuts or cracking skin at corners of mouth
- Redness around mouth
- Dry mouth or cottony feeling in mouth
- Slightly raised bumps resembling cottage cheese
- Loss of taste
In rare but severe cases, oral thrush can spread into the esophagus and cause painful swallowing. Having an weakened immune system increases your risk.
You should see a gynecologist or doctor if you are experiencing symptoms of a yeast infection. Your doctor can rule out other conditions and provide guidance for treatment.
Antibiotics Most Likely to Cause Yeast Infections
Some antibiotics are more likely to cause yeast infections than others. Broad-spectrum antibiotics, which are used to target and kill a wide variety of bacteria, increase your risk the most. They can disrupt the balance of good and bad bacteria in the body and create an environment where yeast infections can occur.
Broad-spectrum antibiotics are extremely common and used to treat a spectrum of infections. Examples of broad-spectrum antibiotics include:
- Penicillins: These antibiotics are widely used to treat a range of infections such as skin infections, urinary tract infections, and chest infections. Examples of penicillins include penicillin, amoxicillin, co-amoxiclav, flucloxacillin and phenoxymethylpenicillin.
- Tetracyclines: These medications are commonly used to treat acne and other skin conditions. However, tetracyclines can also be prescribed to treat urinary tract infections, sexually transmitted infections, eye infections, and gum disease. Other names for tetracyclines include tetracycline, doxycycline and lymecycline.
- Quinolones: These medications are widely prescribed to treat respiratory infections like pneumonia, some skin conditions, and complicated or difficult-to-treat urinary tract infections. Types of quinolones include ciprofloxacin, delafloxacin, gemifloxacin, levofloxacin, moxifloxacin, and ofloxacin.
- Macrolides: These antibiotics are used primarily to treat chest and lung infections. They are a good alternative for people who are allergic to penicillin and can also be used to treat strains of bacteria that are resistant to penicillin. Macrolides are also called azithromycin, erythromycin and clarithromycin.
Taking antibiotics does not guarantee that you will get a yeast infection. However, they can be a side effect, especially with broad spectrum antibiotics. If you are taking a broad spectrum antibiotic and prone to yeast infections, it is important to talk to your doctor. You can then both watch for symptoms and, if needed, promptly start antifungal treatment to ease any discomfort.
Who Is Most at Risk?
Yeast infections are common and can affect anyone. However, some people are more at risk than others. Factors that may increase your risk of developing a yeast infection include:
- Antibiotics: Taking antibiotics can kill good bacteria in the body which allows excess yeast to grow.
- Pregnancy: The hormonal changes that occur throughout pregnancy can disrupt your vaginal microbiome and encourage yeast to grow.
- Oral contraceptives: Taking hormonal birth control can disturb your body’s natural flora and promote excess candida growth.
- Weakened immune system: A weakened immune system or being immunocompromised increases your risk of candida overgrowth.
- Uncontrolled Diabetes: Poorly controlled diabetes can cause fluctuations in blood sugar, which can interfere with your body’s natural flora and encourage yeast growth.
- A history of yeast infections: People with a history of yeast infections are more likely to develop subsequent ones in the future.
How to Prevent a Yeast Infection While Taking Antibiotics
The key to preventing a yeast infection is maintaining a healthy balance of good and bad bacteria in the body and reducing factors that increase yeast overgrowth. Since antibiotics can disrupt your microbiome, it is essential to do what you can to reduce moisture in the affected areas and prevent creating an environment where candida can grow.
You can achieve this through good hygiene and being mindful of certain triggers. Some preventative measures you can take include:
- Wear loose fitting pants and undergarments
- Wear natural fiber
- Promptly change out of wet clothes or bathing suits
- Wash underwear in hot water
- Eat a healthy, well-balanced diet
- Take probiotics during and after your antibiotic course
- Avoid scented feminine products
- Avoid douching
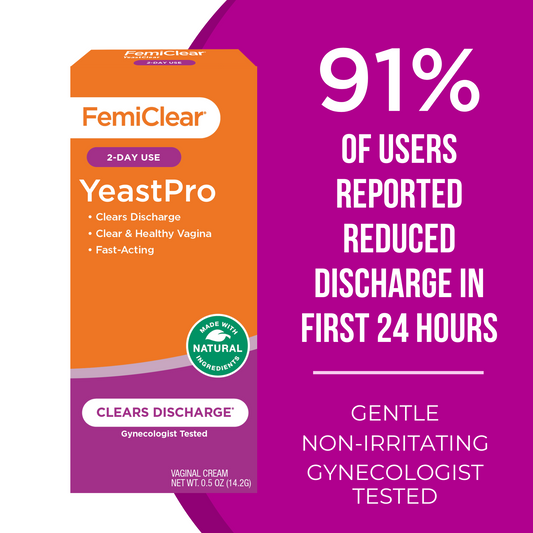
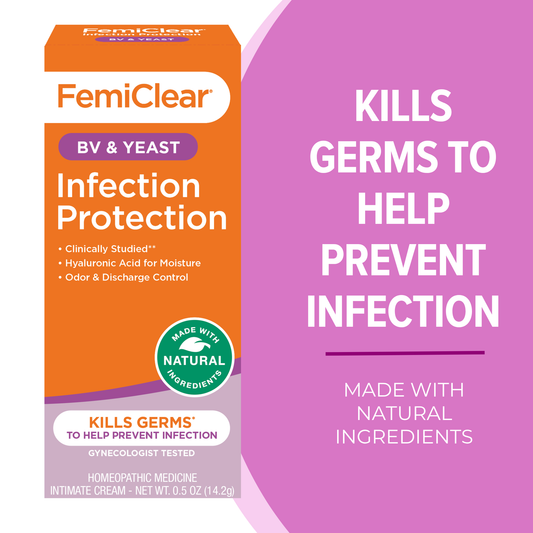
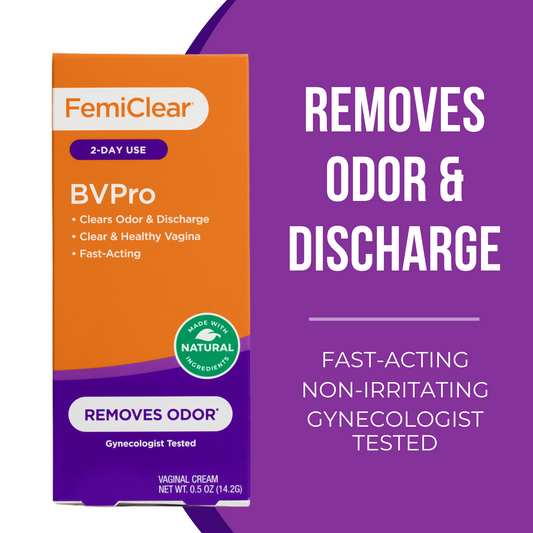
There are also over-the-counter products available that can reduce your risk of getting a yeast infection. Femiclear offers creams that provide yeast infection protection while you complete your antibiotic treatment.
If you are prone to yeast infections or have a history of yeast infections while taking antibiotics, it is important to tell your doctor. They can prescribe an oral antifungal medication called Diflucan, also known as fluconazole, that can prevent yeast infections while you finish your antibiotic course.
If you get a yeast infection while taking antibiotics, you can take an over-the-counter antifungal medication that contains miconazole or clotrimazole. Treatment typically lasts one to seven days. It is also crucial to refrain from any sexual activity while treating your yeast infection. Sexual activity can irritate the affected areas and make your infection worse.
Conclusion
The link between antibiotics and yeast infections is strong but seldom discussed. Antibiotics, while excellent for fighting a wide range of bacteria, can also wipe out healthy bacteria in the body. This can interfere with your body’s natural flora and create an environment where candida, the bacteria that causes yeast infections, can grow out of control.
The type of antibiotics that increase your risk of a yeast infection the most are broad-spectrum antibiotics like penicillins, tetracyclines, macrolides, and quinolones. You can lower your risk by practicing good hygiene and reducing moisture in the potentially affected areas. Your doctor may also prescribe an antifungal medication if you have a history of yeast infections.
In addition, Femiclear is here for you with products that can help prevent yeast infections and soothe any symptoms.
Frequently Asked Questions
Can antibiotics cause a yeast infection?
Yes. Antibiotics can disrupt the balance of good and bad bacteria in your body, allowing Candida to overgrow and cause a yeast infection. This can happen during or shortly after your antibiotic course.
How soon after taking antibiotics can a yeast infection start?
Symptoms can appear while you’re still taking antibiotics or within a few days to two weeks after finishing them. Timing varies based on the antibiotic type, dose, and your individual microbiome.
Which antibiotics are most likely to cause yeast infections?
Broad-spectrum antibiotics (e.g., penicillins, tetracyclines, macrolides, and quinolones) carry a higher risk because they target a wide range of bacteria, including beneficial strains that help keep yeast in check.
How can I prevent a yeast infection while on antibiotics?
Support your microbiome and reduce moisture: wear breathable fabrics, change out of wet clothes promptly, avoid scented products, and consider probiotics. Some people use preventive antifungals under a doctor’s guidance. See prevention ideas in our guide to yeast infection causes.
Do probiotics help prevent antibiotic-related yeast infections?
Probiotics can help maintain a healthy balance of bacteria, which may reduce risk. Look for strains commonly used for vaginal health (e.g., Lactobacillus species). Talk to your provider about timing probiotics during and after your antibiotic course.
What are the signs of a vaginal yeast infection versus oral thrush?
Vaginal yeast infections often cause itching, redness, and thick, white “cottage cheese-like” discharge. Oral thrush can cause creamy white patches on the tongue/cheeks, soreness, and trouble swallowing. Learn more about symptoms and when to see a doctor here.
Can I treat an antibiotic-related yeast infection at home?
Many mild infections can be treated with over-the-counter antifungals (e.g., miconazole, clotrimazole). If symptoms persist, recur, or are severe, see a healthcare provider to confirm the diagnosis and discuss options like fluconazole.
Is it safe to have sex while I have a yeast infection?
It’s best to avoid sexual activity until treatment is complete and symptoms resolve. Sex can irritate inflamed tissue and may prolong recovery.
What if I get recurrent yeast infections after antibiotics?
Recurrent infections (≥2 in 6 months or ≥3 in a year) should be evaluated by a clinician to rule out underlying factors (e.g., uncontrolled diabetes) and discuss preventive strategies.
Are there products that can help while I’m on antibiotics?
Some products are designed to help protect the vulvar area and support comfort while you complete your prescription. Explore yeast infection protection creams and our yeast infection collection.
Oct 26, 2025
Yeast Infection + Itch Relief - 2 Day Dose | Ointment
Kills over 99% of Tough to Treat Yeast*
Learn More