Table of Contents
Table of Contents
Why you should see a Gynecologist
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Jan 03, 2023

What is a Gynecologist?
While many people are familiar with routine healthcare visits to a primary care clinician, not all realize that a gynecologist (GYN) is a vital part of the core medical team for persons with a female reproductive system. A GYN is a medical doctor who specializes in the diagnosis and treatment of conditions and diseases affecting the reproductive system, such as vaginal or pelvic infections, menstrual cycle issues like endometriosis, ovarian cysts, and uterine fibroids to name a few. Some GYN doctors are also obstetricians (OB) who additionally, or exclusively, specialize in the diagnosis, management, and treatments involving pregnancy and delivery.
One of the main responsibilities of a GYN is to diagnose and treat reproductive health conditions. This involves obtaining a full medical history, conducting physical and, at times, internal pelvic exams, ordering and interpreting lab tests, and using medical imaging techniques such as ultrasound and MRI to assess the health of the reproductive organs. Gynecologists also perform surgeries, such as laparoscopies and hysterectomies, to treat conditions affecting the female reproductive system.
As part of the core healthcare team, GYNs also provide preventive care to their patients and, occasionally, may be the only point of contact for many persons within the healthcare system. Routine GYN care includes :
- Conducting regular Pap smear screenings to detect early signs of cervical cell abnormalities or cancer
- Sexually transmitted infection screening and treatment as well as prevention counseling
- Contraception counseling to help prevent unwanted pregnancies
- Menopause symptom screening and management
- Sexual health safety and guidance
- Fertility planning, screening, and guidance
As part of their training, GYNs also learn about the mental and emotional health impact of conditions affecting the reproductive system. They can provide support and counseling to patients confronted with issues such as depression, anxiety, and post-traumatic stress disorder (PTSD), as well as guidance to address any psychological concerns related to reproductive health.
When, and how often, should you see a GYN?
As part of your core medical team, it is generally recommended that you have a routine annual visit with your GYN. . However, there are many reasons why a person might visit a gynecologist, which may vary depending on age.
When should teenagers see a gynecologist?
The guideline association for OB/GYNs, the American College of Obstetricians and Gynecologists (ACOG), recommends having a consultation visit between the ages of 13 and 15. This recommendation is based on the fact that many teens start to go through puberty around this age range. Puberty is a major life transition for our bodies and seeing a GYN allows for a personalized conversation to address questions or concerns about menstrual cycles, sexual health, and overall reproductive health.
Establishing a relationship with a GYN early on can allow teenage patients to feel comfortable discussing health concerns they may have as they get older and can be an important part of developing a healthy relationship with their bodies as well as understanding their reproductive health.
When and how often should adults see a gynecologist?
As part of your routine health maintenance and complete preventative care, it is recommended to have a GYN checkup and STI screen annually. Current cervical cancer screening guidelines advise Pap smears to be performed every 3-5 years starting at age 21. Important to note, however, is that an increased screening frequency may be advised depending on your specific results and plan determined with your GYN clinician.
For patients in their reproductive years, visiting a GYN can help to identify and manage any issues that may arise with the menstrual cycle, pelvic organ health, fertility, or any potential health issues that may impact reproductive health. As patients enter the menopause transition, a gynecologist can help to diagnose and manage symptoms such as irregular or heavy periods, hot flashes, mood swings, and vaginal dryness. A GYN can also guide good pelvic and sexual health maintenance as patients age.
Seeing a GYN is especially important for those who are sexually active, as your clinician can provide guidance on preventing sexually transmitted infections (STIs) and can perform screenings and treatments. STI screening is generally recommended annually or can be more frequent depending on sexual activity as well as the number of partners encountered. Some patients may need to see a GYN more frequently depending on their individual health needs and risks. It is always best to talk to your doctor about how often you should schedule checkups and screenings based on your individual needs.
What types of symptoms require going to a GYN between routine checkups?
Outside of a routine visit or known condition-related issue, many symptoms warrant a GYN visit. Some of the most common symptoms include:
- Unusual vaginal discharge, color, consistency, or odor
- Vaginal or vulvar itching, burning, or irritation
- Vaginal or vulvar pain
- Vaginal or vulvar lumps, bumps, or rashes
- Vaginal dryness
- Painful intercourse
- Pelvic pain or bloating, especially recurrent or persistent
- Breast pain, lumps, or nipple discharge
- Abnormal vaginal bleeding
- Irregular, heavy, painful, or missed menstrual cycles
- Menopausal symptoms, such as hot flashes
What are the most common causes for some of these symptoms?
The top 3-4 common symptoms listed above typically result from an inflammation of the vulva and/or vagina, a condition referred to as vulvovaginitis. This inflammatory response represents an imbalance of the normal bacteria and yeast that make up the vaginal ecosystem and can result from many causes, including:
- Infections
- Recent antibiotic use
- Hormonal changes, e.g. during pregnancy, breastfeeding, or menopause
- Douching
- Spermicide use
- Sex
Vaginal infections are extremely common, with non-STI vaginal infections reported to occur in 1 in 3 persons with a female reproductive system. Some of the most common vaginal infections include yeast, bacterial vaginosis (BV), and genital herpes. There are also many other less common infections for which a GYN visit is recommended to obtain a pelvic exam, with a full STI screening and assessment, especially if you have not experienced symptoms before.
Yeast Infections
Yeast infections, also known as candidiasis, are responsible for approximately one-third of all vulvovaginitis cases in reproductive-age patients, with 70% reporting candidiasis in their lifetime! Although native to the vaginal ecosystem, candidiasis results from the overgrowth and infection with Candida species, typically C. Albicans, that causes symptoms. Typically, a yeast infection will produce a thick, “cottage cheese”-like discharge that can have a white or even green tinge. Common symptoms reported by patients experiencing candidiasis may include itching, burning, swelling of the vagina and/or vulva, painful intercourse, external pain with urination, or even external cuts on the vulva.
Bacterial Vaginosis
BV is the most common cause of vaginal symptoms amongst patients with a female reproductive system, regardless of sexual activity. It results from an overgrowth of one, or several, bacteria that are naturally occurring in the vaginal ecosystem, similar to the process of a yeast infection. Accordingly, the Centers for Disease Control and Prevention (CDC) reports that 84% of patients found to have BV do not report symptoms at the time of diagnosis. When symptoms do result from BV, they frequently include increased thin watery discharge that may be grey or green with a strong fishy odor. The odor may be stronger during periods or after sex. Vaginal itching, burning, irritation, or discomfort with urination may also occur in association with BV.
Genital Herpes
Herpes is one of the most common sexually transmitted infections. It is caused by 2 types of herpes simplex virus, type 1 (HSV-1) and type 2 (HSV-2) which are transmitted through vaginal, anal, or oral sex as well as through contact with the skin or saliva of a person with herpes. The CDC estimates about 1 in 6 people between ages 14 and 49 has HSV. Most people with herpes may have mild or no symptoms at all, but HSV can produce painful blisters or sores around the genital area or mouth which can be particularly noticeable during an “outbreak.” The herpes blisters may take a week or more to heal and flu-like symptoms, such as a fever, body ache, or swollen glands, may occur during the first HSV outbreak.
Which symptoms can be treated with over-the-counter (OTC) vs a prescription?
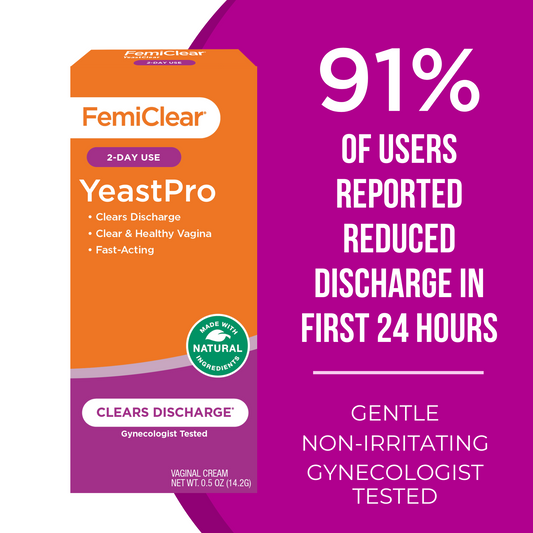
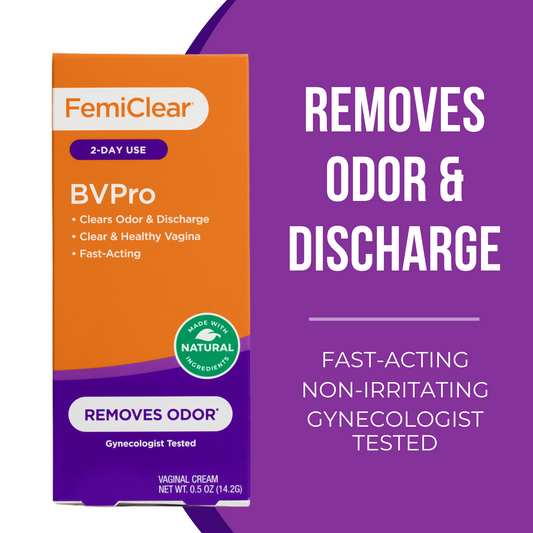
Symptoms such as vaginal itching, odor, or abnormal discharge are commonly due to the most typical causes of vulvovaginitis, like yeast infections and BV. They can often be relieved with OTC products, such as antifungal vaginal creams or ovules for yeast infections, and vaginal gels or suppositories for BV. FemiClear offers both Yeast Infection and Bacterial Vaginosis symptom relief products.
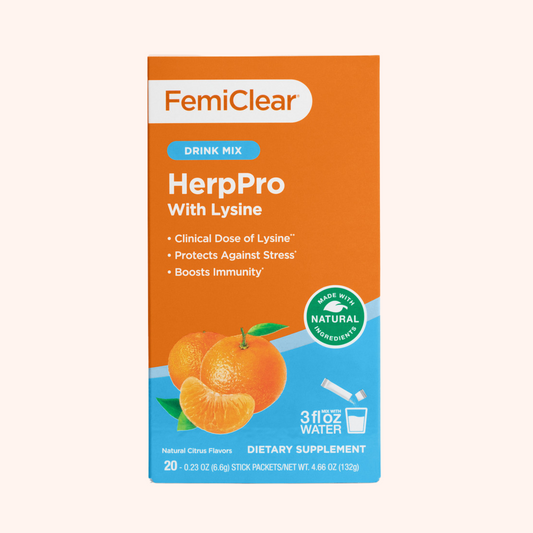
Herpes, on the other hand, is a viral infection that, unfortunately, cannot be cured. OTC medications are not available to treat the cause of herpes but available remedies, such as FemiClear’s Multi-Symptom Relief product, could help you manage the severity of symptoms after being properly diagnosed. It is important to see a GYN for a proper diagnosis as well as to discuss treatment options. They may prescribe antiviral medications to help prevent outbreaks and control the symptoms of herpes.
If you have never experienced symptoms before, or do not experience relief with an OTC product, it is important to see a GYN to confirm the diagnosis and ensure that you are using the appropriate remedy for you.
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Jan 03, 2023
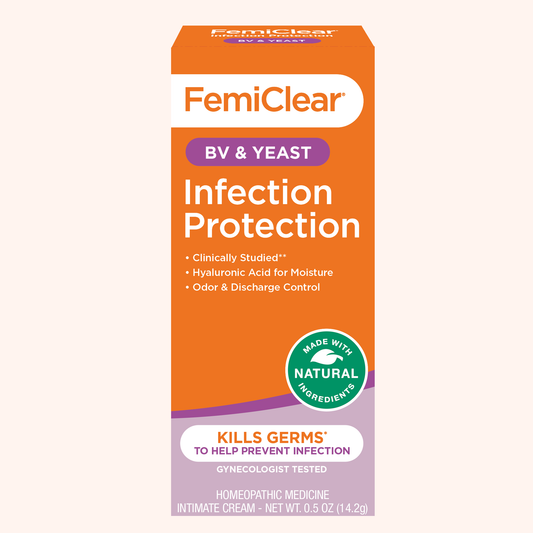
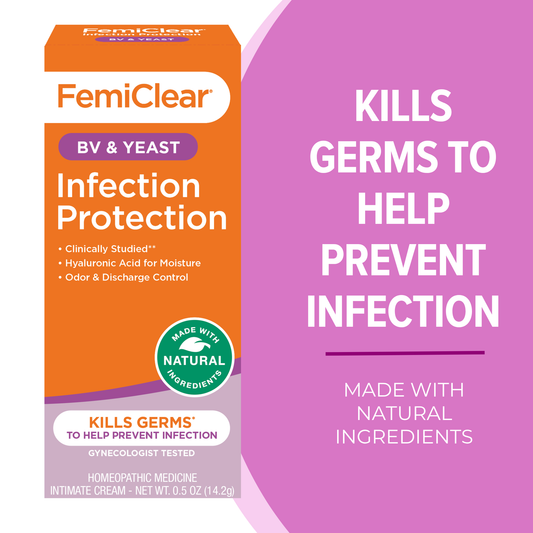
UTI Infection Protection Vulva Cream
Stop infection before it starts
Learn More