Table of Contents
Table of Contents
Women Get Real on How BV Affects Their Lives (Plus, an OBGYN’s POV)
Written by Carrie Murphy, Doula Mar 22, 2023

Bacterial vaginosis is a common vaginal infection that affects 21.2 million women in the US. It’s often asymptomatic, but if you’re someone who does experience symptoms of BV, you know how annoying they can be. Bacterial vaginosis comes with a fishy odor, white, gray or green discharge, and itching.
These symptoms occur most often because of an overgrowth of the bacteria called Gardnerella vaginalis. While this bacteria is always present in the vagina, bacterial vaginosis happens when Gardnerella vaginalis grows too much and overtakes the other healthy bacteria. This is connected to vaginal pH, as well—when the acidity of the vagina drops from its normal 3.8-4.5, that’s when the opportunity for Gardnerella to take hold presents itself. And voila…here come the symptoms.
If you’ve had BV, you’re certainly not alone. We spoke to eight women about their experiences with BV—everything from how this vaginal infection affects their sex life to their self-esteem. Their quotes illuminate some of the causes of bacterial vaginosis, how it feels to have symptoms, and what it’s like to live with a recurrent case of BV. Dr. Melissa Walsh, an OBGYN in Coral Springs, Florida, also weighs in on the real ways that this condition can affect people: medically, mentally, and more.
Bacterial Vaginosis Symptoms
“The two most common symptoms I experience when I have BV are excessive discharge and fishy odor. I go through about 4 pairs of underwear a day when I have an active infection. Typically, I can feel BV approaching by the amount of discharge. To me, BV discharge feels like the gush of blood you experience during your cycle when you sneeze. I can always tell the difference between regular discharge and BV.”—Danielle Stokes, TikTok influencer with over 790,000 followers.
Dr. Walsh says these symptoms are in line with what happens for most women when they get bacterial vaginosis: “The thin and watery discharge may be grey or green with a strong fishy odor. The odor may be stronger during periods or after sex. Vaginal itching, burning, irritation, or external vaginal or vulvar discomfort with urination can also occur in association with BV.”
Sex and BV
“It’s affected my sexual life because I can’t make love in confidence especially when I think it’s me being wet as f when really it’s just the discharge.” —Brittany
“I don’t feel sexy when I have a pungent scent going on and it makes me reject my partner because I’m rejecting myself until I feel it's ‘fixed.’” -Deonjanae
“I got BV after losing my virginity at 18. Not only was I sore, I also smelled like fish and was so uncomfortable. It made me feel gross about myself.” —Anonymous
It’s quite common to get BV after a sexual experience (because of how the act of sex can affect the pH balance of the vagina). This may be more common in women who have penis-in-vagina intercourse, as one 2020 study in the journal Frontiers in Cellular and Infection Microbiology found. The researchers found that the microbiome of the penis can affect the vaginal microbiome, as 31% of the women in the year-long study developed BV. This was more common in women with male partners who were uncircumcised.
Some people are prone to getting BV often after sex, while others only experience it every once in a while. According to Dr. Walsh, “BV is extremely common, affecting up to 60% of sexually active persons, but also occurring in those who are not sexually active. Though not the only cause, sex can be a risk factor for BV because of the impact of a partner’s body fluids on the vaginal discharge bacterial composition.”
Life and BV
“I’m very insecure about things that many women find normal like oral sex, dancing, bending over, going to the bathroom etc. It's not that I experience symptoms that are still affecting my day to day but, I mentally deal with the aftermath of experiencing BV for so long.”—Danielle Stokes
“I was unaware of what BV was until I was diagnosed with it. I went to the doctor as I was feeling unwell and thought I might have a UTI. I was diagnosed with both a yeast infection and BV. Had I known what it was I might have been able to know the symptoms sooner or how to limit my chances of getting it”—Kait
“My BV is triggered by stress and binge eating sugary foods. Mentally and sexually, it’s embarrassing.”—Deonjanae
“I am deeply in love with being a woman, but some parts I could do without...like BV. It sneaks up at the worst time and leaves me feeling less than my best. Dating makes me anxious enough without it, so add in some BV and you might as well just punch me in the face. It can seriously disrupt the flow of life.”—Emily Gay, TikTok influencer with over 8k followers
Having bacterial vaginosis, whether you get it occasionally or have a recurring case, can affect so much more than your actual vaginal health. Many of the women we spoke to clearly expressed how both the lack of discussion and knowledge about the condition, the actual symptoms, and the social stigma of vaginal infections shape their day-to-day experiences.
For Dr. Walsh, this is reflected in the patients she sees and treats for the condition: “Many patients describe a disruption in their day-to-day because of the symptoms and emotional impact of dealing with BV. Through my clinical experience, my patients have taught me that recurrent BV can particularly affect how they see themselves and how they perceive others may see them, which in turn affects so many aspects of their lives, from intimacy to socializing to their level of comfort in the workplace bathroom.”
There’s also a stigma around discussing the condition, something Dr. Walsh says can really affect people’s lives as well. She is hopeful, though, that this is beginning to change: “Social media has provided a platform for people confronted with BV to attest to that and encourage discussion. We need to normalize the conversation around the conditions our reproductive health systems experience so we can have a better general understanding and maybe even better solutions to address these under-discussed, and sometimes under-researched, common medical issues.”
Recurrent BV
“It actually didn't start until I gave birth to my son. It seems to constantly recur and I don't know why which makes it very frustrating. Both my doc & OB don't seem to really have the answer to why it is happening or how I can stop it.”—Kaila
“When I experienced recurring BV, I had it consistently for about 6 years. I was in and out of the doctors at least twice a month until I learned to cope with it by doing things to help minimize symptoms.”—Danielle Stokes
“I have recurring BV, my ex would ask me why I keep getting it and I honestly didn't know what I was doing wrong or if it was him that was throwing my pH off. I've had to go through countless gel and pills as well. I constantly have to use boric acid. It also is very uncomfortable.”—Si
Recurring BV is more common than you think—up to 58% of women get BV again within a year after treatment with oral antibiotics, according to research published in the Journal of Infectious Disease. Women with this issue are very much not alone, as Dr. Walsh emphasizes:
“When patients are dealing with recurrent BV, it’s important for them to know how common it is and how it can happen to anyone, oftentimes spontaneously, especially because our bodies change as we age and go through different phases in life. “
If you have recurrent BV, Dr. Walsh says it’s important to work closely with your care provider to figure out what’s causing your BV. “If you are experiencing recurrent BV, it is helpful for yourself and for whichever clinician you see to keep a brief record of what treatments you’ve been prescribed or tried OTC as well as your menstrual cycle around the time of the BV episode. More information is always better, so including diet, exercise, stressful events, soap/detergent changes, and any change in sexual partner(s) could also help you to target your trigger. This can help to decrease the episode frequency, as a consistent pH is restored through treatments and/or lifestyle changes.”
BV Treatment
“The typical treatment you will receive from a medical provider is an antibiotic. Most come in gel and pill form. I prefer gel (I hate taking pills🤮). Another option that became popular over the last few years is boric acid. There isn't much long-term research on boric acid and reproductive health but people are finding it to be effective. Boric acid is great for infections here and there but if your infections are reoccurring, it is likely boric acid will not fix it. You have to balance your pH.”—Danielle Stokes
“One doc told me it will solve itself, but also gave me medication that helps to get rid of it. But no doctor has really tried to give me more permanent treatment or get to the bottom of why it's happening. I have tried natural vaginal suppositories but the 6-night treatment is $25 and I don't want to have to do that for the rest of my life, since my BV seems to flare up right after my period and sometimes after sex.”—Kaila
“Having multiple trips to the doctor a year-every few months to get the same prescription filled. Subconsciously, I’m just like leave it for me to refill. I’m tired of coming back and explaining my vagina to run tests and be told I was correct—I just wanna fix it at home without a medical professional looking at all my business.”—Deonjanae
“[I dislike] needing to get the test done before being treated even with symptoms and history of recurring BV. Also, the medication makes your stomach upset and gives you a weird taste in your mouth”—Si
Oral antibiotic pills or vaginal antibiotic gels areis the most common line forms of treatment medication for BV. Metronidozole and clindamycin are often prescribed, according to the CDC. As some women expressed above, having to make an appointment to see a clinician can make it hard to actually get these treatments. For people who experience recurrent BV, seeing a medical provider repeatedly is another barrier. Some people may be sensitive to antibiotics and find that taking them over and over also throws off their vaginal microbiome, making them more prone to yeast infections.
Dr. Walsh is sympathetic to all the barriers to BV treatment women experience, from lack of treatment options to general misunderstanding of the recurrent version of BV. She says, “Many patients with recurrent BV commonly go to a number of clinicians and, particularly, if they have never seen that clinician before, they may keep receiving the same prescribed treatments like antibiotic gels or pills.”
As for the boric acid some women have tried to help their BV, she advises: “Boric acid vaginal suppositories are a treatment option commonly used in vaginal infections because they acidify the vaginal environment to help decrease the overgrowth of yeast or bacteria. Their effectiveness for BV, however, is less well studied and is typically used with an oral antibiotic at the same time.”
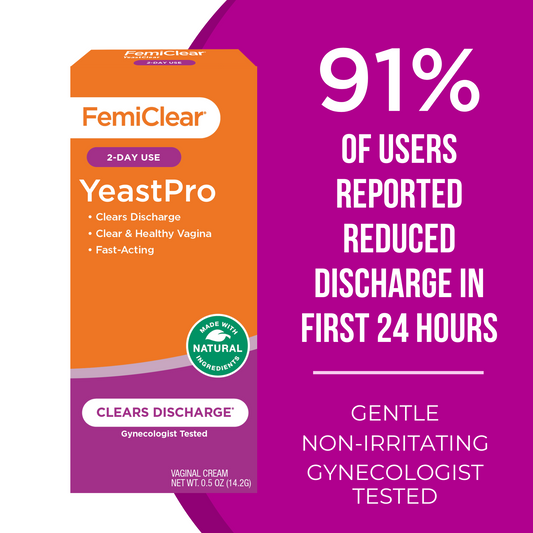
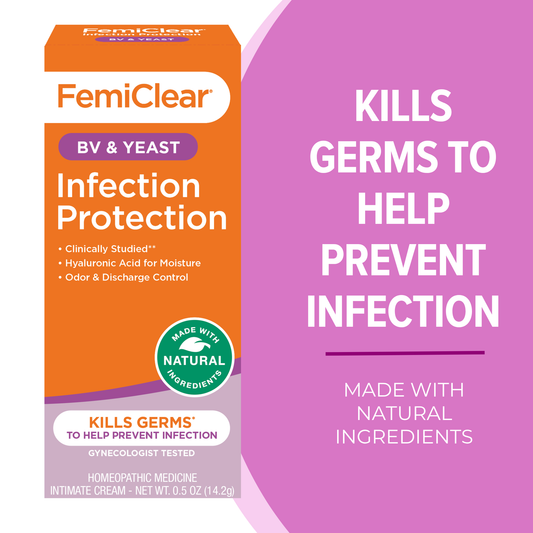
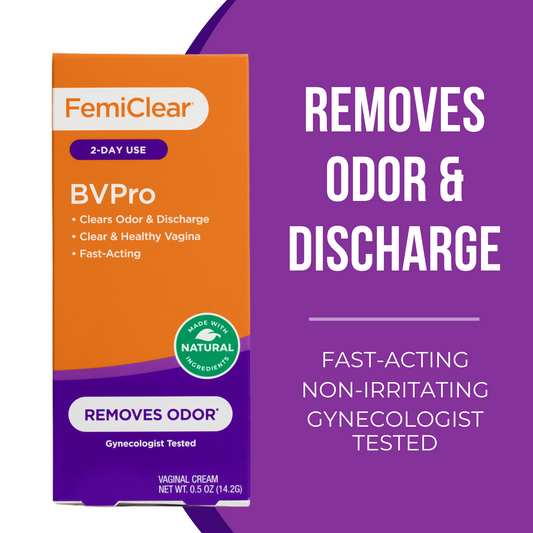
There have been limited over-the-counter options to help women deal with the symptoms of bacterial vaginosis—until now! Here at FemiClear, we have developed a powerful vaginal ointment to help relieve the fishy odor, excessive discharge and vaginal itching that comes along with BV. Our clinical studies show that this product, which works using a two-day dose, reduces up to 99% of Gardnerella vaginalis. 83% of users reported relief from symptoms in the first 24 hours of use, and 91% reported that symptoms were eliminated. **
If you experience discomfort from BV symptoms, FemiClear’s Bacterial Vaginosis ointment may make a difference in your experience of the infection. Dr Walsh adds that other OTC products like FemiClear’s feminine wash and probiotics can help balance your pH and decrease the frequency of episodes as well.
*An independent accredited lab performed an in vitro (non-human/non-animal) time-kill study to measure the amount Gardnerella Vaginalis that was killed. An overgrowth of Gardnerella Vaginalis, can cause a bacterial vaginosis (BV) infection, but might not be the only cause. Data on file.
**As self-reported in a comprehensive IRB-approved study of >100 women. Individual results may vary. Data on file.
Written by Carrie Murphy, Doula Mar 22, 2023
BVPro for Vaginal Odor | Cream
Relief from Odor and Discharge in 24 Hours
Learn More