Table of Contents
Why Does FemiClear Burn?
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Feb 28, 2023

Non-STI vaginal infections occur in 1 in 3 persons with a female reproductive system. Some of the most common vaginal infections include yeast, bacterial vaginitis (BV), and genital herpes. Symptoms, their onset, and intensity will vary by the individual, but there are some symptoms that can linger on or even only start after beginning treatment like the dreaded experience of vaginal burning. This intense and often painful sensation happens to many people for a number of reasons in the setting of an infection as well as its treatment.
What is the true cause of the burning sensation?
To truly understand why we have a burning sensation during infections and during treatment, we need to understand our bodies at a deeper knowledge level. Learning more about how the body works is a tool that can be especially helpful for those who are confronted with recurrent vaginitis, formally diagnosed as 3 infections or more in a year!
The genital area of the female reproductive system has an abundant blood and nerve supply to support its numerous necessary functions for our body’s health and balance. The vaginal tissue, or mucosa, that is part of this system contains different cell types which can be influenced by our nutrition, stress responses, and hormonal signals received through our blood’s circulation, as well as environmental exposures from infections or chemicals in the products we use.
The vaginal mucosa is the first line of defense against many infections because it has multiple tools at its disposal. It has the ability to rapidly shed affected cells, which produces the increased discharge experienced by some people. It contains receptors that enable an immune system respond to foreign bacteria or yeast. And most importantly, the bacterial microbiome contained within the mucosal layer maintains the vagina’s normal acidic pH which discourages and helps to prevent some bacteria or yeast from surviving to cause an imbalance or infections.
During an ongoing vaginal infection, unfortunately, these mechanisms become overwhelmed and the mucosa is stripped of its defense layer. Without those protections, the mucosal tissue becomes very fragile and enters a cycle of inflammation. So, when we experience a burning sensation during treatment for a vaginal infection like BV or yeast, or during a herpes outbreak, that feeling results from the inflammation of the sensitive vaginal mucosal tissue and can extend externally to the labia. Often the pelvic exam for many patients presenting with this symptom in the setting of a vaginal infection, with or without a recent treatment attempt, redness, swelling, and micro tears will typically occur at the transition area from the vaginal mucosa to the labial skin.
When we use a prescribed treatment for infection and/or use an OTC product to help our body restore itself, these products can be associated with a brief episode of vaginal burning. This concurrent episode of burning occurs as the treatment takes effect on the cause of the infection and helps your body to rebalance its pH. While the push for a pH shift toward the normally acidic environment of the vagina starts to occur in the treatment course, the mucosal inflammation, swelling, and microtears, if present, will also be starting their healing process. However, these processes are not synced so this irritating symptom may occur for some.
Is there a difference between the cause of burning from a yeast or BV infection?
In general, the most common vaginal infections, like yeast and BV, cause inflammation in a very similar way. Yeast infections are caused by an overgrowth of Candida yeast in the vagina. They occur in approximated 17-39% of patients with symptoms. BV is the most common vaginal condition amongst those with a female reproductive system, according to the CDC. It is caused by an imbalance in the normal microbiome of the vagina, leading to an overgrowth of one or several bacteria.
The presence of yeast or bacterial overgrowth impacts the pH of the vaginal discharge, commonly making it less acidic and more prone for other infections to occur or intensify. These changes can disrupt the vaginal mucosa’s ability to maintain a balanced environment, which as detailed above, can lead to a cycle toward increasingly severe levels of inflammation of the mucosal tissue as well as the skin of the labia and surrounding genital area. Initiating a prescribed or OTC remedy can be associated with burning at first, but the intensity of that burning should decrease over the course of the first day into the second day of treatment. If you note an increasing intensity or continued discomfort after 2 days of treatment, it is recommended to contact your GYN office for personalized evaluation and treatment planning.
How is burning from a herpes outbreak different?
Herpes is one of the most common sexually transmitted infections which unfortunately cannot be cured. It is caused by 2 types of herpes simplex virus, type 1 (HSV-1) and type 2 (HSV-2) which are transmitted through vaginal, anal, or oral sex as well as through contact with the skin or saliva of a person with herpes. The CDC estimates about 1 in 6 people between ages 14 and 49 has HSV.
During a herpes outbreak, many people will have painful blisters, or small open sores, around the genital area or mouth. Depending on the area where the sores appear, a burning sensation may occur even prior to starting any treatment. The pain and burning felt from HSV blisters or sores on the vulva and external genital skin is caused by the exposure of underlying layers of the skin by the sores and can be worsened by friction from the movement against your clothes, towel, sheets, etc. Applying an ointment or cream to the affected areas may incite further burning depending on the chemicals used and particularly, how raw the sores are at the time of application. If the HSV sores occur in the area of transition from the labia to the mucosal tissue of the vagina, a similar cycle of inflammation as described previously may occur. Unfortunately, the herpes virus can also hide within the vulvovaginal tissues and cause recurrent outbreaks, leading to further inflammation cycles in previously inflamed areas. OTC medications are not available to treat the cause of herpes but available remedies, such as FemiClear’s Multi-Symptom Relief product could help manage the severity of symptoms. It is important when using any topical product for herpes symptom relief, to wash your hands thoroughly after application to reduce transmitting HSV to other parts of your own body or others.
Is there a way to help, or even prevent, that burning sensation?
Not everyone experiences a burning sensation with vaginal infections or treatments, but for those who do, it can be quite disruptive to their daily activities. The longer you have symptoms of a vaginal infection or outbreak developing, the more time there is for the inflammatory response of the mucosal and surrounding tissues to intensify. Time is really of the essence when it comes to treating vaginal infections, herpes outbreaks, and any condition that affects the female reproductive system.
Primary prevention by maintaining a healthy active lifestyle, self-care aimed to decrease stress, as well as nutrition and hygiene practices to help your body maintain your pH balance, are our core tools. Unfortunately, there are no guaranteed remedies that will completely prevent the risk of a burning sensation associated with treatment but there are several methods to help decrease the intensity of it! Some methods and lifestyle adjustments to try when you’re experiencing these symptoms:
- Gently wash the external genital area with lukewarm to cool water and pat dry before using any product or prescription
- Use a gentle, unscented feminine wash, like FemiClear's, externally if desired
- Apply a cold compress to the affected area before and after treatment
- Avoid wearing tight-fitting clothes frequently, especially during treatment
- Avoid and stop douching
- Avoid intercourse until your symptoms resolve
- Probiotics may also play a role in helping your body to rebalance
OTC products such as bacterial vaginosis cream can help soothe the sensation but different remedies work for different people. Pain targeting OTC topical medications, like those that contain the numbing agents, benzocaine or lidocaine, can contain additives that can worsen or prolong the discomfort associated with vaginal infections. It is also important to avoid exposure to alcohol-based or heavily fragranced products as these can exacerbate your symptoms.
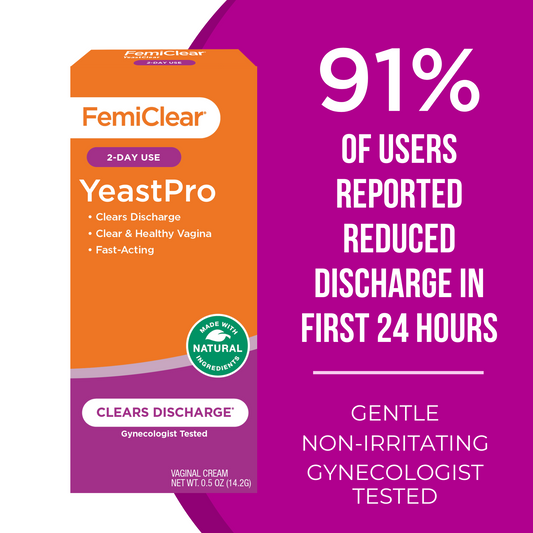
For burning associated with moderate to intensely symptomatic yeast infections, the application of a natural remedy, like FemiClear’s 2 Day Dose Yeast Infection, may help to decrease your symptoms quicker. If you are experiencing a burning sensation for more than 2 days after starting a treatment, which includes the day you start, or if you feel you need to take medication specifically for the intensity of pain or discomfort, then an in-person visit for an exam, or at minimum a televisit, could be indicated and we recommend contacting your GYN physician.
Resources:
Nguyen JD, Duong H. Anatomy, Abdomen and Pelvis, Female External Genitalia. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK547703/
Balakrishnan SN, Yamang H, Lorenz MC, Chew SY, Than LTL. Role of Vaginal Mucosa, Host Immunity and Microbiota in Vulvovaginal Candidiasis. Pathogens. 2022 May 25;11(6):618. doi: 10.3390/pathogens11060618. PMID: 35745472; PMCID: PMC9230866.
Anderson DJ, Marathe J, Pudney J. The structure of the human vaginal stratum corneum and its role in immune defense. Am J Reprod Immunol. 2014 Jun;71(6):618-23. doi: 10.1111/aji.12230. Epub 2014 Mar 24. PMID: 24661416; PMCID: PMC4024347.
Vaginitis in Nonpregnant Patients. American College of Obstetrics and Gynecology, Practice Bulletin Number 215, January 2020. Reaffirmed 2022.
Bacterial Vaginosis (BV) Statistics. CDC. Accessed 2/5/2023
Genital Herpes – CDC Basic Fact Sheet. CDC. Accessed 2/7/2023
Herpes Simplex – Emedicine, MedScape. Ayoade F, et al. Medscape. Accessed 2/7/2023
Written by Melissa Walsh, MD, FACOG Board-certified OB/GYN Feb 28, 2023
BVPro for Vaginal Odor | Cream
Relief from Odor and Discharge in 24 Hours
Learn More